Over the last few years, a growing community of detransitioners has formed online. Despite the visibility recently given to the topic in mainstream media, including a recent 60 Minutes episode featuring detransitioners and their stories, detransition is still a poorly understood phenomenon. A recent exploratory cross-sectional study aims to serve as a springboard for further academic research on the subject. It focuses particularly on uncovering the specific needs that detransitioners experience and the support - or lack thereof - that they receive.
|
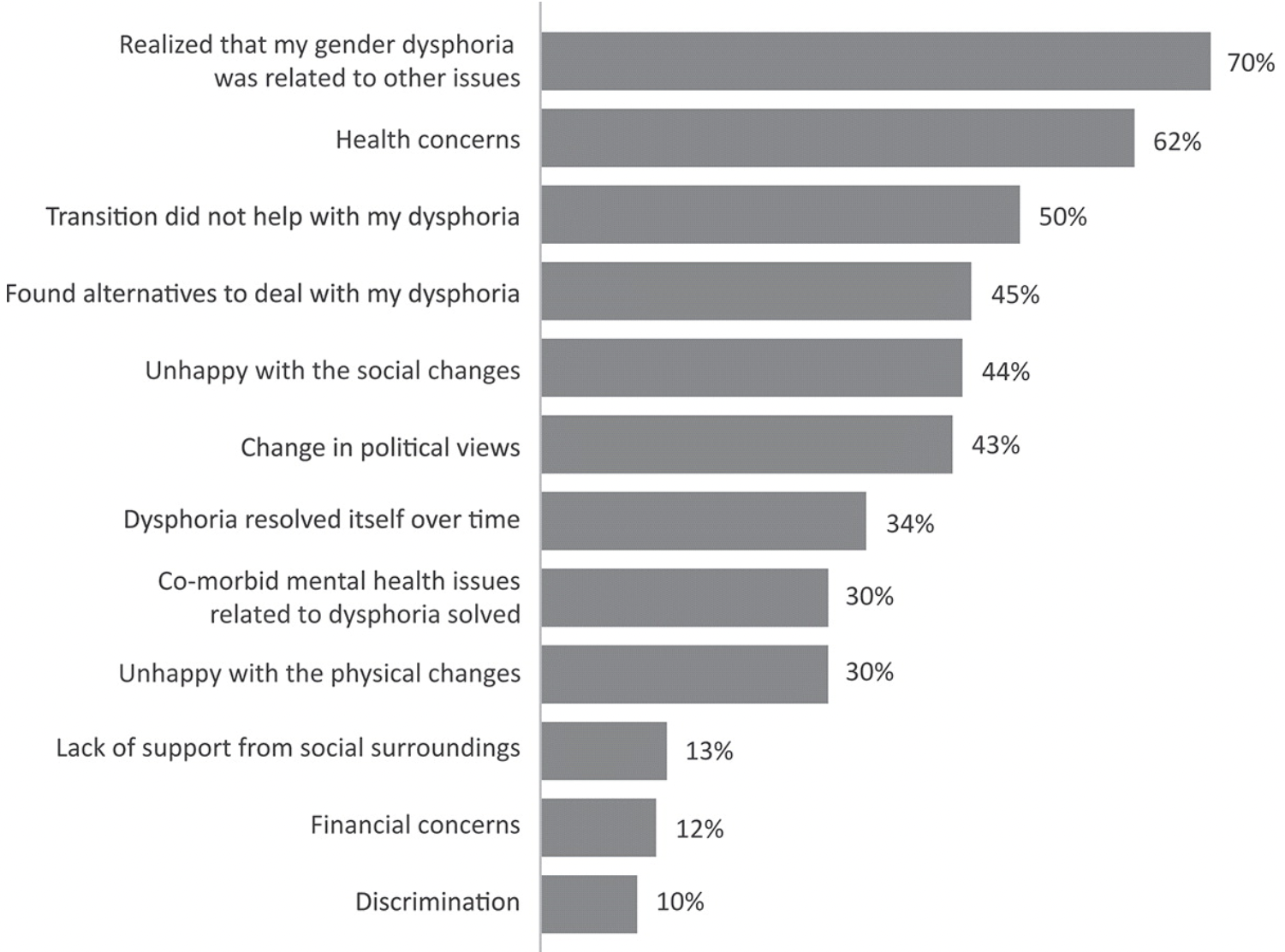
Among the total of 237 survey participants, 92% were birth-registered females. Approximately 2/3 had transitioned both socially and medically, while just under 1/3 transitioned only socially (the option of "only medical" transition was not provided in the survey responses). Among those who medically transitioned, 46% underwent "gender-affirming" surgeries (vs. only undergoing hormonal interventions). The average age of transition was 18 for social transition (17 for females, 24 for males), and 20.7 for medical transition (20 for females, 26 for males). A quarter of the respondents began medical transition before 18. The average age of detransition was 23 (22 for females, 30 for males). On average, detransition occurred roughly 5 years after transition was initiated (with males taking somewhat longer to detransition). The participants' decision to detransition was most often tied to the realization that their gender dysphoria was related to other issues (70%), health concerns (62%), and the fact that transition did not alleviate their dysphoria (50%). Interestingly, over 4 in 10 (43%) participants endorsed a change in political views as a reason for detransition. |
Reasons for Detransitioning
Figure 1. Reasons for detransitioning (n=237). Vandenbussche E (2021). |
Most participants reported significant difficulties finding the help that they needed during their detransition process from medical, mental health, or LGBT communities. Only 13% of the respondents received help from LGBT organizations when detransitioning, compared to 51% when transitioning. A number of participants reported negative reactions from LGBT and medical communities, and 51% of the sample expressed that they did not feel supported during their detransition.
Most detransitioners reported ongoing needs related to managing comorbid mental health conditions (65%), finding alternatives to medical transition (65%), and coping with regret (60%). Half of the sample reported the need for medical information on stopping or changing hormone regimens. A great majority of participants also expressed the need to hear about others' detransition experiences (87%) and getting in contact with other detransitioners (76%). The study highlights the urgency of providing appropriate medical, psychological, legal, and social support to detransitioners.
This is the first large-sample, peer-reviewed study of the experiences of individuals who identify as detransitioners. Another study earlier this year also attempted to examine detransitioner experiences, but it used a sample of individuals who self-identified as transgender, non-binary, or as "cross-dressers." That study suggested that the leading reason for their detransition was external pressure. In contrast, this most recent study of individuals who explicitely identify as "detransitioners" suggests a strong influence of internal, rather than external, factors. The marked difference in the findings between these two recent studies, both of which use convenience online samples, highlights how the choice of sample may impact study applicability.
As the numbers of transitioners have sharply grown in the last 5 years, and as transition eligibility has become far less restrictive, it is inevitable that the number of detransitioners will grow. It is vital that health systems begin to track detransition in order to better understand the trajectories of gender dysphoric youth. It is also critical that gender medicine practitioners develop treatment protocols to help detransitioning individuals with significant unmet mental and physical health needs.
To full text of the publication is available here.
If you would like to read more about the phenomenon of detransition, we recommend the following sources:
Boyd, I., Hackett, T., & Bewley, S. (2022). Care of Transgender Patients: A General Practice Quality Improvement Approach. Healthcare, 10(1), 121. https://doi.org/10.3390/healthcare10010121
Cohn, J. (2023). The Detransition Rate Is Unknown. Archives of Sexual Behavior, 52(5), 1937–1952. https://doi.org/10.1007/s10508-023-02623-5
D’Angelo, R. (2020). The man I am trying to be is not me. The International Journal of Psychoanalysis, 101(5), 951–970. https://doi.org/10.1080/00207578.2020.1810049
Entwistle, K. (2020). Debate: Reality check – Detransitioner’s testimonies require us to rethink gender dysphoria. Child and Adolescent Mental Health, camh.12380. https://doi.org/10.1111/camh.12380
Expósito-Campos, P. (2021). A Typology of Gender Detransition and Its Implications for Healthcare Providers. Journal of Sex & Marital Therapy. https://www.tandfonline.com/doi/abs/10.1080/0092623X.2020.1869126
Hall, R., Mitchell, L., & Sachdeva, J. (2021). Access to care and frequency of detransition among a cohort discharged by a UK national adult gender identity clinic: Retrospective case-note review. BJPsych Open, 7(6), e184. https://doi.org/10.1192/bjo.2021.1022
Jorgensen, S. C. J. (2023). Transition Regret and Detransition: Meanings and Uncertainties. Archives of Sexual Behavior. https://doi.org/10.1007/s10508-023-02626-2
Levine, S. B. (2018). Transitioning Back to Maleness. Archives of Sexual Behavior, 47(4), 1295–1300. https://doi.org/10.1007/s10508-017-1136-9
Littman, L. (2021). Individuals Treated for Gender Dysphoria with Medical and/or Surgical Transition Who Subsequently Detransitioned: A Survey of 100 Detransitioners. Archives of Sexual Behavior, 50(8), 3353–3369. https://doi.org/10.1007/s10508-021-02163-w
MacKinnon, K. R., Kia, H., Salway, T., Ashley, F., Lacombe-Duncan, A., Abramovich, A., Enxuga, G., & Ross, L. E. (2022). Health Care Experiences of Patients Discontinuing or Reversing Prior Gender-Affirming Treatments. JAMA Network Open, 5(7), e2224717. https://doi.org/10.1001/jamanetworkopen.2022.24717
Marchiano, L. (2021). Gender detransition: A case study. Journal of Analytical Psychology, 66(4), 813–832. https://doi.org/10.1111/1468-5922.12711
Pazos Guerra, M., Gómez Balaguer, M., Gomes Porras, M., Hurtado Murillo, F., Solá Izquierdo, E., & Morillas Ariño, C. (2020). Transsexuality: Transitions, detransitions, and regrets in Spain. Endocrinología, Diabetes y Nutrición (English Ed.), 67(9), 562–567. https://doi.org/10.1016/j.endien.2020.03.005
Roberts, C. M., Klein, D. A., Adirim, T. A., Schvey, N. A., & Hisle-Gorman, E. (2022). Continuation of Gender-affirming Hormones Among Transgender Adolescents and Adults. The Journal of Clinical Endocrinology & Metabolism, dgac251. https://doi.org/10.1210/clinem/dgac251
Turban, J. L., Loo, S. S., Almazan, A. N., & Keuroghlian, A. S. (2021). Factors Leading to “Detransition” Among Transgender and Gender Diverse People in the United States: A Mixed-Methods Analysis. LGBT Health, 8(4), 273–280. https://doi.org/10.1089/lgbt.2020.0437
Vandenbussche, E. (2022). Detransition-Related Needs and Support: A Cross-Sectional Online Survey. Journal of Homosexuality, 69(9), 1602–1620. https://doi.org/10.1080/00918369.2021.1919479